Diabetic Retinopathy

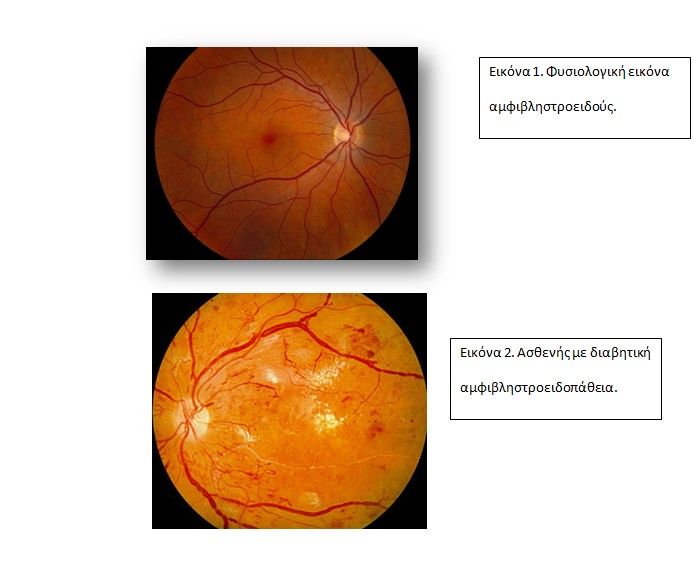
Diabetic retinopathy occurs in 40% of patients with diabetes mellitus. It usually affects the central retina, called the macula or the periphery. It occurs more often in patients with type 1 diabetes rather than type 2.
What are the risk factors?
- Duration of diabetes mellitus
- Poor blood sugar regulation
- Pregnancy
- Hypertension
- Kidney disease (due to diabetes)
- Other causes: hyperlipidemia, smoking, obesity, anemia.
Mechanism of pathogenesis:
- Destruction of capillary pericytes => thickening of capillary endothelial cells => obstruction.
- Destruction of the inner blood-retinal barrier (inner BRB).
- Destruction of cells by entry of sorbitol and increase in oxidative stress => Increase in cell permeability.
- Neovascularization due to a decrease in the supply of oxygen to the retinal tissue, with an increase in VEGF factors, the creation of shunts between vessels and finally the appearance of neo-vessels.
What categories does it fall into?
- Mild Non- Proliferative Diabetic Retinopathy (Mild NPDR): Occurrence of microaneurysms and hemorrhages.
- Moderate Non-proliferative Diabetic Retinopathy (Moderate NPDR): Significant hemorrhages in 1 to 3 quadrants or mild IRMA.
- Severe Non- Proliferative Diabetic Retinopathy (Severe NPDR): Significant bleeding in all 4 quadrants, IRMA, venous beading.
- Productive retinopathy (PDR): Occurrence of neovascularization of the optic nerve or in the periphery of the retina.
- End-stage diabetic retinopathy: Vitreous hemorrhage, and tractional retinal detachment.
- Diabetic macular disease: It is the entity in which macular edema occurs due to diabetic disorders in the central area of the retina (fovea) and which very soon creates symptoms on the patient’s vision.
- Ischemic type diabetic macular disease: observed in long-term existence of macular disease and is due to the absence of good blood supply to the macula and the foveal area. (Enlarged foveal avascular zone).
What are the main symptoms?
- Blurred vision appearance of floaters due to vitreous hemorrhage.
- Deep pain upon the appearance of neovascularization of the iris and is due to increased intraocular pressure.
- Focusing disorders due to blood sugar disorders (transient hyperopia) due to disorders of the intraocular lens of the eye
- Absence of symptoms!!! Early or moderate diabetic retinopathy may not give sufficient symptoms.
What is the procedure during the diagnosis?
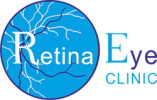
The main method of diagnosing the condition is with dilated fundus exam. Many auxiliary imaging tests are now at our disposal to facilitate the diagnosis.
It is a good practice to take annual photographs of the fundus of the eyes to monitor and stage the disease. We also routinely perform macular OCT to screen for diabetic macular edema, as well as fluorescein angiography when we suspect proliferative diabetic retinopathy.
What is the treatment followed to treat the condition?
The treatment depends on the stage of the retinopathy and ranges from simple monitoring to emergency surgery.
Macular disease is now primarily treated with repeated use of intravitreal anti-VEGF injections with very good results. Complementary laser treatment in several cases is necessary. Especially in proliferative diabetic retinopathy pan retinal laser photocoagulation is very important in managing the disease.
Vitreous hemorrhage combined with tractional retinal detachment is a relatively urgent situation which frequently requires surgery.