What should we know?
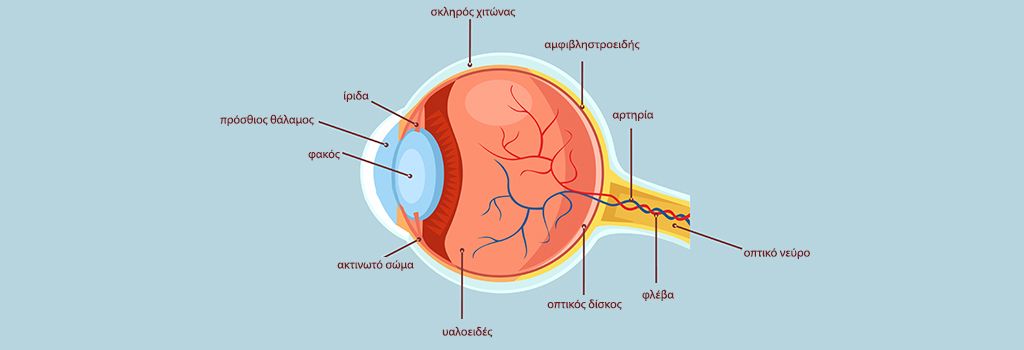
In 50% of the population, by the age of 50, the vitreous, the jelly inside the eye, begins to detach from the retina. This is known as vitreous detachment.
In some cases, however, the adhesions of the vitreous to the retina are very strong, resulting in partial detachment of the vitreous and traction on the retina. This is a very undesirable condition because this traction causes a decrease in central vision and can lead to further problems such as macular hole, macular membrane and cystoid edema.
Patients with vitreous traction should be thoroughly examined by a specialist ophthalmologist because they often have peripheral retinal tears that go undiagnosed and can lead to retinal detachment. Retinal detachment is very dangerous, because it can lead to blindness.
What are the symptoms of the condition?
The most common symptoms patients present are:
1) reduced visual acuity and blurred vision
2) illuminations, i.e. flashes
3) micropsia, where objects appear smaller than the pathological eye
4) metamorphosis, where lines appear distorted instead of straight.
In some cases, metamorphopsia is the first symptom and the most important before the decrease in visual acuity.
How is vitreous traction syndrome diagnosed?
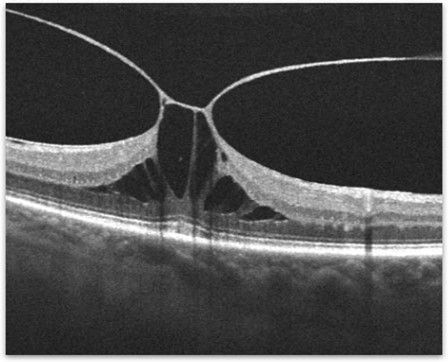
Optical coherence tomography (OCT) is the most common examination performed for the diagnosis and monitoring of patients. This is a technology that provides us with cross-sections of the retina and the vitreous surface. Thus, in great detail we can examine abnormalities on the vitreoretinal surface.
Figure 1. OCT of a patient with severe vitreous traction and cystic retinal edema. |
What is the treatment for vitreous traction syndrome?
There are 3 main treatment options for vitreous traction syndrome.
- Careful monitoring of patients at regular intervals with OCT. This mainly concerns asymptomatic patients whose central vision has not yet been affected.
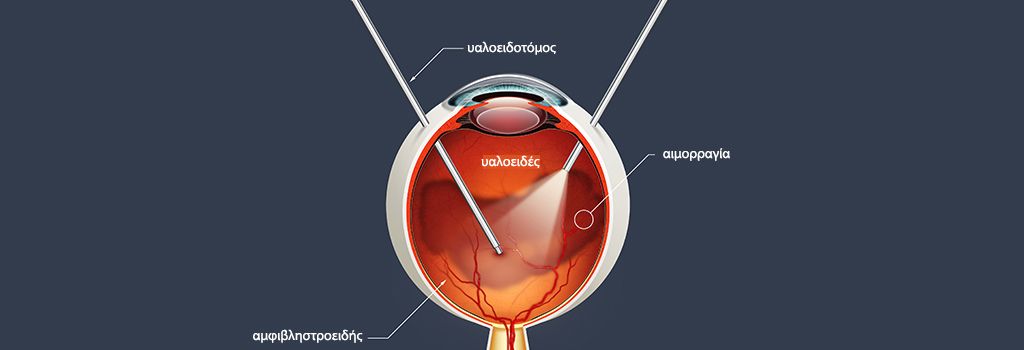
- For patients whose central vision has been significantly affected, the main treatment is surgery. The surgery is called vitrectomy or vitrectomy. The surgery involves the surgical removal of the vitreous through microscopic trocars (25g) in the white part of the eye (sclera). Some studies have shown that the sooner the surgery is done, the better the recovery of vision.
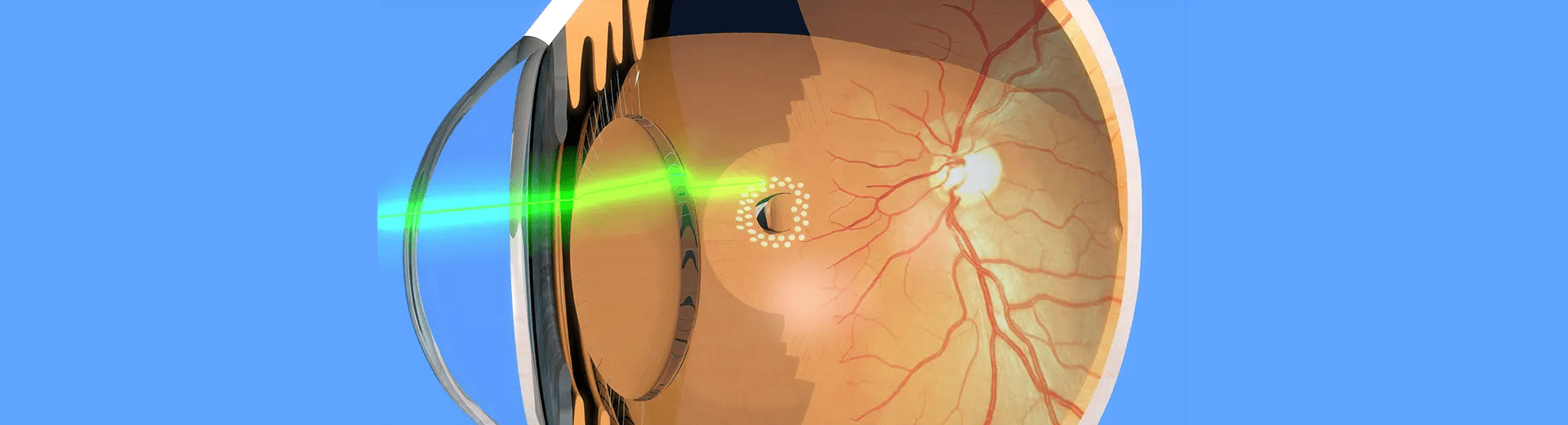
- Pneumatic vitreolysis- a small bubble of gas is injected into the eye. Then we ask the patient to look down several times an hour for 1 to 2 days. Thus, the continuous movement of the bubble within the eye releases the pull of the vitreous on the retina and macula.
Most patients with vitreous traction maintain good vision even if treatment is needed. Contact specialist ophthalmic surgeon Georgios Trichonas to learn more about your treatment options.